The rate of FEV1.Spirometry: normal indices
Spirometry is designed to assess the state of the lungs of a person. The procedure pursues a number of clinical goals, including assessment, training and diagnostic. This study is assigned for the detection of lung pathologies of various genesis, monitoring the patient's condition and evaluating the therapeutic effectiveness of the treatment. In addition, spirometry is used to teach a person the right respiratory technique. The scope of this type of research is quite wide. In this article, we will consider the procedure for spirometry, indications, contraindications and the features of its use.
What is the standard FEV1, consider in this article.

Indications
The human breathing system consists of three main elements:
- Respiratory paths that allow air to pass into the lungs.
- Pulmonary tissue that promotes the exchange of gases.
- The chest is inherently a compressor.
The failure of at least one of these elements inhibits the functioning of the lungs. Spirometry allows assessing respiratory parameters, diagnosing existing pathologies of the respiratory tract, describing the severity of the disease and whether the prescribed therapy is effective.
The rate of lung capacity is of interest to many.
Indications for the appointment of spirometry are:
- Respiratory diseases of a regular nature.
- Cough in chronic form, shortness of breath.
- In addition to other examinations of the respiratory tract in the diagnosis of pulmonary pathologies.
- Finding the causes of failure in gas-exchange processes in the body.
- Assessment of the risks of prescribed therapy in the treatment of lungs and bronchi.
- Detection of signs of airway obstruction( in case of smoking patients) in the absence of severe symptoms of this pathology.
- General characteristics of a person's physical condition. What is the volume of maximal ventilation of the lungs, consider below.
- In preparation for surgical intervention and lung examinations.
- Diagnosis of early stages of chronic obstructive pulmonary disease, development control and evaluation of further prognosis.
- Determination of the degree of destruction of respiratory function in tuberculosis, bronchial asthma, bronchoectatic disease, etc.
- Diagnosis of restriction.
- Allergic reactions( especially those with an asthmatic character).

All of the above cases are the reason for the appointment of spirometry. This type of research is not widespread, many people simply do not know about it. However, it is very popular in such medical fields as allergology, pulmonology and cardiology. Coupled with spirometry, the patient can be directed to the dynamometry, which determines the strength of the pulmonary muscles. Here, the peak exhalation rate is detected.
The main value of spirometry, otherwise known as the external respiration function or FVD, plays in the diagnosis of chronic obstructive pulmonary disease and asthma. Experts advise to pass a test for ventilation of the lungs regularly in the event that a patient has one of the above pathologies. This will help to prevent the occurrence of concomitant complications.
The table of normal spirometry parameters is presented below.
General information
The FVD is performed using a spirometer. This is a special device that can read lung indicators during a functional examination. With its help, it is also possible to stimulate the respiratory function. This is especially true for patients who underwent surgery on the lungs and who have certain problems with the work of the respiratory system.
Types of spirometry
Spirometers come in many forms, including:
- Computer. Equipped with ultrasonic sensors. It is called the most hygienic spirometer. Has a high accuracy of indicators, because it contains a minimum of internal parts.
- Plethysmograph. This is a special chamber where the patient under examination is located, and special sensors transmit the indicators. This type of spirometer is considered the most accurate at the moment.
- Water. It does not apply to ultra-precise spirometers, but the measurement range is quite wide.
- Dry mechanical. The device is rather small, while reading the information it can at any position of the patient. The range of action is rather small.
- Stimulating or motivating.
The methods of the procedure are also different. Breathing can be examined at rest, or an accelerated exhalation evaluation is performed, as well as lung ventilation at maximum capacity. The norm of lung volume is indicated by the mean. There is also such a thing as dynamic spirometry, which shows the functioning of the lungs at rest and immediately after physical exertion. Sometimes spirometry with a drug test is used:
- A test with medications - bronchodilators such as "Ventolin", "Salbutamol", "Berodual", etc. Such medicines have an expanding effect on the bronchi and help to identify a spasm in a latent form. Thus, the accuracy of the diagnosis is increased and the effectiveness of the therapy is evaluated. It is important to understand that obstructive pulmonary disease leads to a change in the flow-volume loop.
- Expert provocation test. It is carried out to clarify the asthmatic diagnosis. Such a test is capable of revealing hyperreactivity and the emerging spasm in the bronchi. The test is performed using methacholine, which is inhaled by the patient during spirometry. In the spirometry table, the normal parameters are indicated in great detail.
Additional study of pulmonary diffusion function
Modern spirometric devices allow further investigation of pulmonary diffusion. This refers to the methods of clinical diagnosis. The study assumes an assessment of the quality characteristics of the oxygen supplied to the blood and the carbon dioxide released by inhalation and expiration. If diffusion is reduced, this is a sign of serious pathologies in the function of respiratory organs.
In the field of spirometry, there is another important study called bronchospirometry. This examination is carried out with the help of a bronchoscope and allows assessment of lung and external respiration separately. When bronchospirometry should be administered anesthesia. The examination helps to calculate the vital capacity, minute volume of lungs, respiratory rate, etc.

Preparation and conduct of
To obtain the most accurate results of the study, it is important to prepare correctly for spirometry, especially when performing the procedure in an outpatient setting. Examination of the forced expiratory volume is performed on an empty stomach in the morning, or at another time, but with the condition of skipping meals. If this is not possible, then it is recommended to eat some low-fat in a few hours before the procedure.
Recommendations
There are other recommendations for preparation for spirometry, namely:
- Refuse from smoking before the procedure.
- You can not use toning beverages on the eve of the examination.
- Drinking alcohol before spirometry is also prohibited.
- Sometimes you may need to stop taking certain medications.
- Clothing during the procedure should not impede movement and interfere with breathing.
- Before the procedure, the doctor is required to measure the height and weight of the patient, as these indicators are important for evaluating the results of the study.
- Before starting the procedure, it is necessary to be at rest for about 15 minutes, so you should come in advance. Breathing should be calm.
Spirometry is performed on an outpatient basis. Different methods and types of research suggest different sequences of actions. The algorithm of steps during the survey can also be influenced by the patient's age and general health. If it is a question of spirometry in a child, it is necessary to create comfortable conditions so that the child does not experience fear and excitement. Otherwise, the indicators may be blurred.

Standard conditions
Standard spirometry conditions:
If the patient does not have information about his height and weight, the physician conducts the necessary measurements. On the device, before the procedure begins, a special disposable mouthpiece is put on.
The spirometer program includes information about the patient.
The doctor gives an explanation of how to breathe during the study, how to maximally inhale. The patient's position should be with a flat back and a slightly raised head. Sometimes spirometry is performed in a recumbent or standing position, which is mandatory fixed in the program. The nose is clamped with a special clothespin. The mouth of the patient must fit tightly around the mouthpiece, otherwise indicators may be underestimated.
The study begins with a phase of calm and even breathing. At the request of the doctor, a deep breath is exhaled and exhaled with maximum effort. Further, the air velocity is checked with a quiet expiration. To get the full picture, the breathing cycle is performed several times.
The duration of the procedure is no more than 15 minutes.
Indicators and rate of FEV1
Spirometry provides data on many indicators that have certain norms. Interpretation of the results of the study makes it possible to identify pathologies in the respiratory system and to prescribe the correct therapy. The main parameters of spirometry are:
- .This is nothing more than the vital capacity of the lungs, which is calculated by the difference between the volume of inhaled and exhaled air. This is the actual figure. There are other indicators, except FEV1.
- FVC.Actual vital capacity of the lungs. It is also determined by the difference between the volume of inhaled and exhaled air, but the exhalation in this case should be forced. The norm is 70-80% LIVING.
- Rovd. This is the reserve volume of inhalation. Determines the volume of air that a patient can breathe after a standard inspiration. Norm 1,2-1,5 liters
- Rovyd. Reserve volume of exhalation. This is the amount of air after a standard exhalation. The norm is 1.0-1.5 liters.
- OEL or total lung capacity. Normally, this is 5-7 liters.
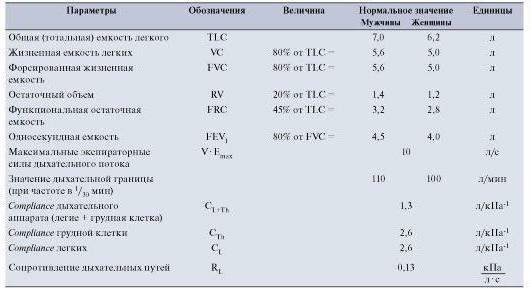
- Norm of FEV 1. Volume of exhaled air at the maximum forcing in the first second. The norm is more than 70% of FVC.
- Tiff. Designed to determine the quality of patency of the respiratory system. The rate is 75%.
- PIC.Volume of air on exhalation. The norm is more than 80% of FEV1.
- MOS.Instantaneous space velocity. This is the speed with which the air flow is exhaled. The norm is more than 75%.
- BH or respiratory rate. The norm is 10-20 respiratory maneuvers per minute.
There are certain features of spirometry in children. The first is age, the child should not be under five. This limitation is due to the fact that at a younger age, the child is not able to make a proper exhalation, which will reduce the rates. Beginning at the age of nine, a child can be examined as an adult. Before this age is reached, it is important to create a comfortable for the baby atmosphere using toys and benevolent treatment. For this reason, spirometry in young children should be carried out in special centers specializing in pediatrics.
Before the procedure it is important to explain to the child how to inhale and exhale. Sometimes for clarification, pictures and photos are used. The specialist should carefully monitor that the lips of the child tightly fit the mouthpiece.
Interpretation of the results
The parameters obtained during spirometry are compared with the norm in view of gender, weight and age. The conclusion on the survey is a graph with an interpretation of the indicators. Explanation on the results can be given by the attending physician.
The following data are decoded:
- Inhaled air volume in milliliters.
- Exhaled volume after the deepest inspiration.
- Gas volume on exhalation.
- The difference between the inhaled and exhaled air volume.
- Speed of exhalation and inspiration.
- Volume of forced exhaled air.
Features of the procedure
Spirometry in adult patients can be performed by a number of specialists, including a pulmonologist, nurse or functional diagnostician. In childhood, the procedure is carried out by a pediatrician. There are also compact spirometers, which make it possible to make the simplest test at home. This is relevant for people suffering from asthma, who need to monitor possible seizures.

Spirometry is a safe procedure and makes it possible to use it without restrictions. Of the side effects can be called mild dizziness during the procedure, but this phenomenon takes place after a couple of minutes.
However, forced inhalation and exhalation can affect intracranial and intra-abdominal pressure, therefore, it is not recommended to perform the procedure after a recent cavitary operation, myocardial infarction, stroke, bleeding of the lungs, pneumothorax, hypertension and poor blood coagulation. Age over 75 years is also a contraindication.
We reviewed the FEV1 norm and other indicators.
